By Howard G. Hindin, DDS
Installment 2 – September 1, 2017
My Journey is to see if I can follow the advice I would offer patients to help them achieve optimal health by addressing the “Four Pillars of Health”.
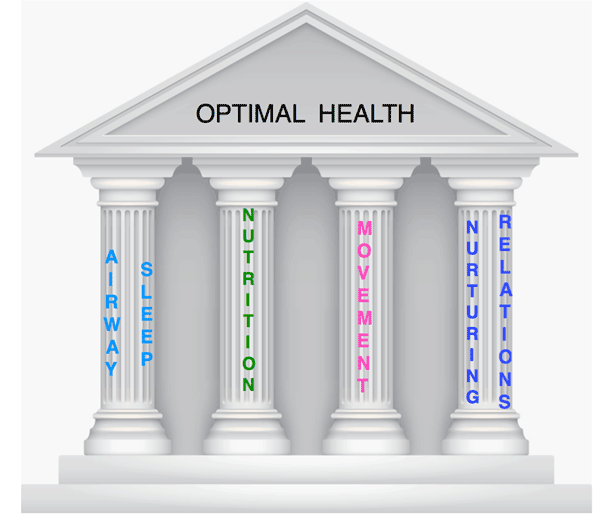
Chronic / acquired diseases are often the result of damage or imbalances occurring to our pillars of health. These imbalances are expressed in different ways at different times in our lives. Without correcting the imbalances, the expressions will keep reoccurring.
I am sharing details and experience of my medical history because I know there are many doctors and patients who are experiencing similar health challenges.
How healthy I can and want to be!

Today, I will share my efforts to improve and restore my Airway/Sleep pillar.
The Past
I am 76 years old and have sleep apnea (for at least 20 years). I developed pulmonary vein stenosis as a result of an ablation to attempt to correct a heart beat irregularity known as atrial fibrillation (AFib). When my AFib started, over 20 years ago, I was unaware of the strong connection between AFib and sleep disordered breathing.
My episodes of irregular and rapid heart rate occurred almost exclusively at night, arousing me from sleep for the rest of the night. Initially, normal rhythm would be restored during the day, especially after vigorous exercise. (I was an adrenaline addict. Activity and stress were good – resting was bad.)
In a short period of time I went from being athletic, running marathons, to shortness of breath and wheezing, to even coughing up blood on slight exertion.
The second ablation, caused scarring around the pulmonary veins (from my left lung to my left heart), resulting in complete blockage. As a result, I was left with no oxygen return from my left lung – which obviously impacted significantly on my quality of life.
Even after the second treatment, my heart rate and rhythm were not normal. It was only after I discovered and addressed my sleep apnea that normal rhythm was restored (along with the help of an innovative cardiologist and medication). Using an oral appliance and/or a CPAP improved sleep, breathing and brought my AHI to normal levels.
What is it like to not breathe well?
Take it from me – you do not know how hard we work to breathe, day and night. When you don’t eat well or exercise enough, you know it, but if you are not sleeping or breathing well, you may not know it.
With pulmonary vein stenosis and reduced oxygen I experience the difference between good and poor breathing on a daily basis. Changes in diet, exercise, stress, weather and general health affect the way I breathe and sleep.
The Present
I advise patients that they should have their sleep appliances checked and sleep tests repeated on a regular basis. Why? Physiology changes. Weight, diet and physical activity will change. Medications are added, altered and eliminated.
Anyone with high blood pressure, high cholesterol or abnormal sugar levels knows the need for regular checkups and medication monitoring. Most sleep patients do not do the same – nor did I.
So, following my own advice, I did a Home Sleep Test (HST) with my sleep appliance (relative little snoring) with a surprising result – an AHI of 22 (moderate sleep apnea). I repeated the HST the following night, wearing my CPAP along with my oral appliance, and measured an AHI of 10.5 (moderate sleep apnea). My CPAP is 8 years old – the mask leaks.
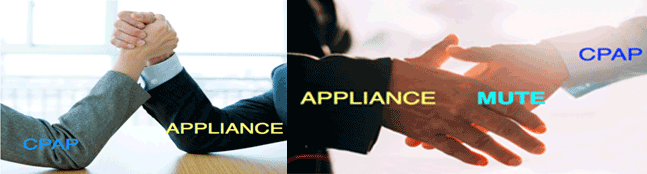
I called Scott Blodgett from ResMed for his thoughts and suggestions. ResMed is a leader in providing both oral and CPAP sleep devices and monitoring equipment. Scott is a big proponent of addressing the needs of the individual patient. We have had discussions about how there should not be a turf war between sleep dentists and sleep physicians. It should not be a question of whether an oral appliance or CPAP mask is better, but rather what will provide the best solution for the individual patient.
Are you an Airway Practitioner? Don’t be a hero. You cannot do the best for your patient by yourself. Collaborate and build an airway team for your patients.
As practitioners we often try to be heroes. Sleep and airway problems are complex and always involve many conditions that need treatment and management. Treatment must be individualized and collaboration is needed for optimal care.
I want to – and will – get my AHI under 5. I have a plan!
I am having my sleep appliances adjusted and tuned using Physiological Monitoring Instrumentation. I have scheduled an overnight PSG and will be updating my CPAP machine and mask.
I had an appointment with Steven Park, an ENT and sleep physician to check my nasal breathing. An examination of my nasal airway showed enlarged turbinate bones, inflammation, and collapse of the nasal walls with increased airway resistance. We discussed surgery, which I am not yet ready to consider. We decided to include the nasal dilator device Mute (RhinoMed) during the PSG to see how that will affect the results.
There are two ways we get the air we need – our noses and mouths. Nasal breathing has physiological benefits. I know my nasal breathing can be better. How? At our AAPMD conference in Tucson last year I had the opportunity to be introduced to RhinoMed, a company that offers a nasal dilator called Mute.
The Mute fits inside the nose and keeps the nose more open. I have been using it since. It improves nasal breathing during exercise and sleep. I find it a wonderful way for patients who are resistant to an ENT referral to assess their nasal breathing.
If I have to use an oral appliance with a CPAP and Mute to breathe better, live longer and stay healthier, I will do it.
There is more to my plan. My airway is even more than my mouth, tongue and nose. I am not a mouth breather nor do I have a restricted lingual frenum, but I will get a myofunctional evaluation to be sure.
Neck, back, rib position and posture also play a role in optimal breathing. Diet, nutrition and weight gain affect breathing, sleep and inflammation. Sleep hygiene, pillows, mattresses and bedroom conditions are also contributors. Reducing stress by improving mindfulness is all part of the plan. I am blessed by knowing many practitioners with expertise in all of the above areas.
Follow me as I share my journey to an optimal airway.
I welcome your comments, your thoughts and most certainly, your support.
American Academy of Physiological Medicine and Dentistry (AAPMD), and the Foundation for Airway Health (FAH), I have strongly advocated an interdisciplinary, collaborative approach for optimal health.
The 2017 AAPMD Airway Summit and the 2nd FAH White Flag Event, along with the American College for Advancement in Medicine (ACAM), will be held in San Juan, Puerto Rico, September 13 – 16. Our meetings focus on “Collaboration for Optimal Health”. So much wonderful information will be disseminated – but can we use what we learn to help our patients AND ourselves?


