By Howard G. Hindin, DDS
Installment 4 – January 12, 2018
Last time I shared my frustrations with getting an overnight sleep test (PSG), to obtain a new CPAP for healthier and more optimal sleep. (See: Would You Follow the Advice You Give to Your Patients – Part III). It was an aggravating, frustrating experience that was so bad it would have been funny if wasn’t my sleep and breathing.
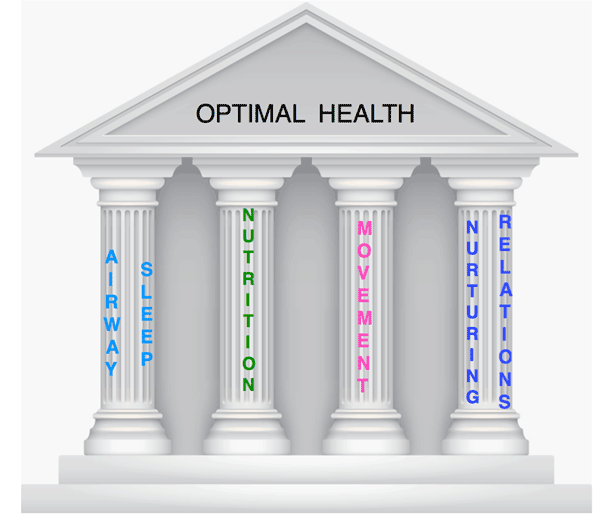
My goal is to be optimally well by strengthening my “Four Pillars of Health”. I do have chronic health issues, expressed in symptoms and testing. My blood chemistry shows evidence of chronic inflammation. I started by looking at my Airway and Sleep Pillar, as they seemed to be most in need of repair.
In the middle of October, I attended the Sleep Education Consortium, 3 days of physicians, dentists and other practitioners learning together to provide a collaborative approach to better serve sufferers of sleep / airway problems. I traveled to Houston to attend where I was invited to speak about the Foundation for Airway Health. It was a wonderful environment of openness, networking and collaboration. It attracted a good mix of physicians and dentists. Neurologist and sleep physician, Jerald Simmons hosted the conference; he is a strong believer in the dentist’s role in treating sleep/airway conditions. He’s been doing it for over 20 years.
 At the invitation of Jerald Simmons, MD, I arrived the evening before the conference to redo my PSG in his sleep lab. This time the test included Esophageal Pressure Monitoring (PES). A thin catheter is inserted through the nose and down the back of the throat into the esophagus to measure negative pressure and air flow limitations.
At the invitation of Jerald Simmons, MD, I arrived the evening before the conference to redo my PSG in his sleep lab. This time the test included Esophageal Pressure Monitoring (PES). A thin catheter is inserted through the nose and down the back of the throat into the esophagus to measure negative pressure and air flow limitations.
Imagine you’re sipping something through a straw and somebody squeezes the straw. That creates negative pressure that pulls in your cheeks. When negative pressure results from a restricted airway, it can cause a sucking in of your cheeks, nasal tissues, throat and even chest walls. One of three things can happen: an apnea event, a hypopnea event or an arousal (you wake up!). The PES instrumentation offers a more complete diagnosis of sleep disorders.
Whichever of these three things does happen, the physiological effect on the body is the same, sympathetic nervous system up-regulation (fight or flight) changes in your nervous system and the consequences.
Houston We Have A Problem – And That’s A Good Thing.
All sleep test experiences are not created equal. In the last episode, I shared how an overnight sleep study (PSG) at a local sleep laboratory failed to show I had a level of sleep apnea to allow me to get a new CPAP. The issue was that I did not sleep and you must sleep to have sleep apnea.
 In Houston, within an hour, there was a sufficient recording of apnea events to fit and titrate a CPAP machine. What was the difference? First, time was spent discussing my history, past studies and current medical conditions and treatment – and customizing the testing and treatment. In my case it was the addition of the PES and medication so I would sleep and register what happens to my breathing when I slept. The result – without the use of a CPAP or an oral appliance I had severe sleep apnea. Now, with that diagnosis, I was fitted and titrated with a new CPAP and different mask utilizing nasal pillows in place of the previous mask.
In Houston, within an hour, there was a sufficient recording of apnea events to fit and titrate a CPAP machine. What was the difference? First, time was spent discussing my history, past studies and current medical conditions and treatment – and customizing the testing and treatment. In my case it was the addition of the PES and medication so I would sleep and register what happens to my breathing when I slept. The result – without the use of a CPAP or an oral appliance I had severe sleep apnea. Now, with that diagnosis, I was fitted and titrated with a new CPAP and different mask utilizing nasal pillows in place of the previous mask.
For me, the nasal pillows were magic, providing so much more comfort. Also, the new machine provides auto-adjustment for airflow differences on inspiration and expiration, shuts off automatically after a few seconds if I go to the bathroom and turns back on when I return to bed and put the pillows over my nose.
 The machine also records information about my sleep that can be sent to my sleep physician. And, the hose is more flexible so it is less of an annoyance. I am both sleeping and breathing better. I do best when wearing an oral appliance along with the CPAP. There will be more to share in the next episode.
The machine also records information about my sleep that can be sent to my sleep physician. And, the hose is more flexible so it is less of an annoyance. I am both sleeping and breathing better. I do best when wearing an oral appliance along with the CPAP. There will be more to share in the next episode.
Some Thoughts About Our Healthcare System
The results of my initial sleep study left me upset and frustrated. I was suffering from sleep apnea, my oral appliances(s) and old CPAP were no longer providing optimal treatment. I knew what I had and what I needed. That of course was my “patient” perspective.
 The “healthcare” system needed to have a diagnosis obtained without the use of a CPAP or oral appliance (baseline), before treatment. If I did not sleep and had no apnea events – then I must not have apnea and did not qualify for treatment or should I say treatment that would not get insurance reimbursement.
The “healthcare” system needed to have a diagnosis obtained without the use of a CPAP or oral appliance (baseline), before treatment. If I did not sleep and had no apnea events – then I must not have apnea and did not qualify for treatment or should I say treatment that would not get insurance reimbursement.
This is an interesting time in healthcare. Practices are merging and being purchased by hospital centers and becoming mega practices. Insurance companies are merging. All are trying to be more efficient and cost-saving. At the same time, the incidence of chronic disease, growth and development problems, and behavior, learning and performance disorders is increasing in epidemic growth. Who is the center of the healthcare system? The Doctor? Insurance Company? Hospital Center? Drug Company? Pick one – It is certainly not the patient.
This is also a time that there is increasing evidence there is hope and treatment for chronic disease. Dale Bredesen’s work with dementia and Alzheimer’s Disease, Brad Bale and Amy Doneen‘s work with cardiovascular disease, as well as other investigators demonstrate the treatment of different chronic diseases is often similar – involving nutrition, sleep, airway and breathing, movement and exercise and nurturing relationships (my pillars of health). Solutions are becoming visible. Let’s put our focus, energy and money there!
Airway / Sleep / Diet / Nutrition

Sleeping and breathing better have been a big boost to my efforts to improve my diet and lose weight. Airway and Nutrition are intimately connected. When there are issues with both it is a “perfect storm”, each feeding the other with worsening function and health. The good news is that when corrected together the benefits potentiate each other.
Let me share with you a little about my recent blood work. It showed increased fasting blood sugar, elevated HbA1C and a poor lipid profile, as well as an increase in C-reactive protein, a common marker for inflammation. I had the signs of a highly stressed system; elevated cortisol levels and insulin resistance. I was becoming diabetic, and increasing my risk for heart disease and other problems.
My sleep and sleep breathing are so much better as I continue to work on the nutritional component. I am attempting to eliminate carbohydrates and especially sugar. I decided I would follow a ketogenic diet and the principles of Dr. Gundry’s The Plant Paradox Diet. Ketogenic diets greatly reduce the amount of carbohydrates consumed so that the body burns fat for fuel instead of carbs. As the fat is broken down for fuel, ketones are produced — hence the name “ketogenic”. This is not a new concept. The ketogenic diet was the treatment for epilepsy prior to the introduction of Dilantin. It is also the diet advocated by the late Robert Atkins. In brief, the principles are: no sugar, no grains, lots of low starch vegetables, reduced protein and high in beneficial fats, especially medium chain triglyceride fat as found in a part of coconut oil (caprylic acid).
Salt is interesting. I am supposed to be on a low salt diet. Carbohydrates cause fluid retention. Where water goes, salt follows. Where salt goes, water follows. With a major reduction in carbohydrates I lost fluids and salt (sodium). As I stay on this diet, I have to be less restrictive about salt intake. In fact, I have to make sure not to be too low on salt intake while observing a ketogenic diet. I picked Dr. Gundry’s version of the ketogenic diet because I liked his evolutionary biology model.
A typical day started with an egg or two, for lunch often an avocado, maybe nuts or cheese and a dose of MCT (caprylic) oil, with some lemon and lime. (Avocado is an excellent anti-inflammatory food).
 Dinner was a big salad with some protein, chicken or fish. After a short time of very low carbs, no wine, no bread, no grains nor desserts, and after grieving their losses and social issues (stares and comments from friends), I noticed I felt better: more energy, more body flexibility, no hunger or cravings and much less aches and pains. The morning walks from my bed to the bathroom used to be painful and noisy as I moaned and bitched about the first movement of the day. That has stopped. I walk up the 22 steps to our door without needing to stop. From the time I started in October until the beginning of 2018, I have lost over 35 pounds.
Dinner was a big salad with some protein, chicken or fish. After a short time of very low carbs, no wine, no bread, no grains nor desserts, and after grieving their losses and social issues (stares and comments from friends), I noticed I felt better: more energy, more body flexibility, no hunger or cravings and much less aches and pains. The morning walks from my bed to the bathroom used to be painful and noisy as I moaned and bitched about the first movement of the day. That has stopped. I walk up the 22 steps to our door without needing to stop. From the time I started in October until the beginning of 2018, I have lost over 35 pounds.
Another feature of this diet is intermittent fasting, allowing 12 hours or more between the last meal of the day and breakfast the next. All I want for lunch is an avocado; that’s it.
I’m approaching 77 years old. I have some chronic health issues that I am told are irreversible (or are they?). But, I look forward to continued improvement. I refuse to be defined by the label that came with the diagnosis.
Can Anyone Have a Life Without Stress?
 The answer is NO. If we are alive there is stress. The goal is not to remove all stress. It is how we manage the stress — or don’t — that affects us. It is how we hold onto things or let go, what we focus on and for how long, that affects our thoughts, our neurotransmitters, biochemistry and physiology.
The answer is NO. If we are alive there is stress. The goal is not to remove all stress. It is how we manage the stress — or don’t — that affects us. It is how we hold onto things or let go, what we focus on and for how long, that affects our thoughts, our neurotransmitters, biochemistry and physiology.
So, at the same time I’m managing my diet, cholesterol levels and glucose levels, I’m also working on mindfulness meditation every morning to manage my cortisol levels and epinephrine levels. Many of us on good diets are not managing our stress and we produce the same biochemistry and physiology our old poor diet did.
So what did I learn from 2017? What I am I looking forward to in 2018?
 I learned that moving toward more optimal health requires a multifaceted approach. It involves work on all of the four pillars of health. It is not easy!!! Progress is not consistent. Knowing what to do is only one part of the solution. There are lots of roadblocks and diversions. I am learning not to get frustrated if I don’t have a good day as long as if at the end of the entire week I feel I did better following my beliefs than I did the week before. (Forgiving my indiscretions keeps my cortisol levels down!)
I learned that moving toward more optimal health requires a multifaceted approach. It involves work on all of the four pillars of health. It is not easy!!! Progress is not consistent. Knowing what to do is only one part of the solution. There are lots of roadblocks and diversions. I am learning not to get frustrated if I don’t have a good day as long as if at the end of the entire week I feel I did better following my beliefs than I did the week before. (Forgiving my indiscretions keeps my cortisol levels down!)
I am really feeling better. Sharing my journey with all of you has helped keep me on track – Thank You All. With knowledge and support you can “Take Charge of their Health”, and will be healthier. I believe these people will change the world for the better. Helping to make it happen is my passion.
I invite you, my readers, to share your own stories. I invite practitioners interested in sharing this journey with me, please contact me. I am thinking of doing workshops together with other practitioners to learn and do this together. Anyone interested? Let’s have healthier doctors for healthier patients.
Looking forward to a happier, healthier 2018!

Join me at:
AAPMD Airway Summit
November 8-10, 2018 Red Rock Resort Las Vegas Nevada
A Unique Event Bringing Together the Meetings of:
AAPMD – ACAM – AAOSH

