By Howard G. Hindin, DDS
Installment 3 – October 11, 2017
The Overnight Sleep Test
In the past, I have joked with friends that I know of a 100% effective cure for sleep apnea – Don’t Sleep! Well, in my case, the joke turned out to be on me…
Two months ago, I began a journey to see if I would be able to completely follow the advice I give my own patients – not partially, but completely. (Note: If you have not been following my experience on this blog, you can read the previous installment.)
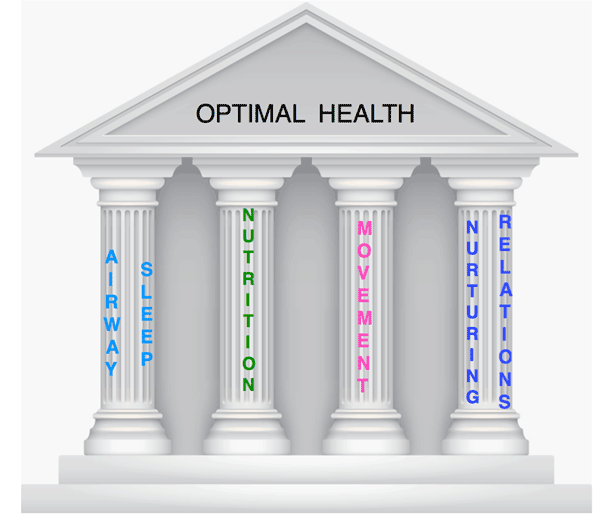
My goal is to be optimally well by strengthening my “Four Pillars of Health”. I do have chronic health issues, expressed in symptoms and testing. My blood chemistry shows evidence of chronic inflammation. I started by looking at my Airway and Sleep Pillar, as they seemed to be most in need of repair.
I have improved the quantity and quality of sleep, and lowered my AHI by adjusting my oral appliance and combining it with the use of my CPAP. Using a nasal dilator (Mute). improved my sleep even more. I had my examination and consult with Steven Park MD, ENT, and scheduled an overnight PSG for the titration (calibration) of a new CPAP machine to use in conjunction with my oral appliance. He had suggested an Auto PAP as this device adjusts to meet my changing airway needs.
 I looked forward to my PSG (overnight, in-lab sleep test) and getting my new, well-fitting and titrated Auto PAOP. The sleep facility was well-furnished with a comfortable mattress and even had a flat screen TV, giving me the chance to watch Monday Night Football while settling in for my night’s sleep.
I looked forward to my PSG (overnight, in-lab sleep test) and getting my new, well-fitting and titrated Auto PAOP. The sleep facility was well-furnished with a comfortable mattress and even had a flat screen TV, giving me the chance to watch Monday Night Football while settling in for my night’s sleep.
I had completed the necessary forms (most of them concerning my insurance coverage and responsibility for payment, rather than my health and sleep history). I had a copy of my prescription from Dr. Park. The plan was to wear the nasal dilator along with the CPAP during the test. That was not to happen that night!
 The sleep lab did not have a documented diagnosis of sleep apnea on file that would satisfy the insurance company for reimbursement, and therefore, would not agree to do the titration. I would have to do a split study where the first part of the night would be sleep with nothing to establish the diagnosis of sleep. Once sufficient data was obtained to confirm the diagnosis, the second part of the night could then be a CPAP titration.
The sleep lab did not have a documented diagnosis of sleep apnea on file that would satisfy the insurance company for reimbursement, and therefore, would not agree to do the titration. I would have to do a split study where the first part of the night would be sleep with nothing to establish the diagnosis of sleep. Once sufficient data was obtained to confirm the diagnosis, the second part of the night could then be a CPAP titration.
Since my original diagnosis of moderate sleep apnea 12 years ago, I have not slept without either an oral appliance or CPAP or both. On my insistence, a phone call was made to a director of the center and yes, I had to have the diagnostic test first. (I had not shared that I was a dental sleep medicine practitioner).
It was a fitful night of poor sleep. Sometime after 3 a.m., I called the Sleep Tech and asked when I would be getting to use the CPAP. I was told I did not pass the “protocol” to allow me to have a CPAP titration. I would need to wait for the test to be interpreted, and then come back for a second night where CPAP titration would be done. The result of the call – I had to do a diagnostic split study test.

When I finally got to speak to Dr. Park and the pulmonologist who reviewed the sleep test, I found that I not meet the protocol, because I no longer had sleep apnea. I had eliminated my sleep apnea – by not sleeping. My AHI score was 1.5. The pulmonologist said I should be happy that I do not have sleep apnea.
When I finally got to speak to Dr. Park and the pulmonologist who reviewed the sleep test, I found that I did not meet the protocol, because I no longer had sleep apnea. I had eliminated my sleep apnea – by not sleeping. My AHI score was 1.5. The pulmonologist said I should be happy that I do not have sleep apnea.
I asked Dr. Park, “Do you believe I no longer have apnea?” He said everything clinically shows I do and he wrote me a prescription so I could purchase an Auto PAP machine, but may not get reimbursement from my medical insurance.How frustrating! I am stuck in the tangled web of the healthcare system. I cannot get the care I believe I need because I did not sleep enough to qualify for a diagnosis of sleep apnea. It may be the first test I ever failed.
Many patients I see do not know they have an airway / sleep problem. It is difficult to get them to accept the idea of their “hidden” airway issue. If a person is overweight or does not exercise, he or she knows it, and cannot honestly deny it. This is not true with sleep / airway problems. I have to convince patients to even investigate a sleep issue and have either a home sleep test (HST) or overnight test (PSG).
The scoring is based on an AHI score. I believe relying on that scoring method alone may miss cases of sleep disorders needing treatment. If the sleep test comes back negative, does it mean the patient is truly OK, or not fully diagnosed? Are patients actually needing treatment neglected because for some reason on the night of their sleep test they did not meet the criteria protocol?
There is no way I can believe I do not have sleep apnea. Without an oral appliance or CPAP, I sleep and breathe poorly and my wife hears me gasping, unable to breathe. So, am I cured? What do I do next?
I had a conversation with Jerald Simmons, MD, a Houston physician who is board certified in neurology, sleep and epilepsy, and a leading educator in the need for protocols and collaboration of physicians and dentists for optimal sleep treatment. He is the founder of the Sleep Education Consortium and newly appointment Board member of the Foundation for Airway Health.
We discussed repeating the PSG and incorporating Drug Induced Sleep Endoscopy, (DISE) to better identify my problem. This week is Dr. Simmons’ annual Sleep Education Consortium (October 12 – 14). I am going to attend and arrive a day earlier to do another PSG in his lab. All sleep labs may not be created equal. I will report on my experience in the next installment.
In the interim, I am working on my other Four Pillars of Health. I will be sharing my efforts in diet and nutrition using a ketogenic diet. (I have lost over 20 lbs. since I started). Why a ketogenic diet?
There is evidence to suggest it helps both weight loss and cognitive function, and the effects of hypoxia. Want to read more? Find out how a collaborative approach may be the answer to protecting our minds. Get a copy of The End of Alzheimer’s: The First Program to Prevent and Reverse Cognitive Decline by Dale Bredesen, MD. More on restoring my nutritional pillar in the next episode.
 Lastly, there is Mindfulness. I have been practicing meditation for over thirty years. I have done it almost every morning and find it very beneficial. The frustration with my sleep testing – not getting my new CPAP – along with the cancellation of the AAPMD meeting in Puerto Rico due to the hurricane, have added more stress and lost sleep.
Lastly, there is Mindfulness. I have been practicing meditation for over thirty years. I have done it almost every morning and find it very beneficial. The frustration with my sleep testing – not getting my new CPAP – along with the cancellation of the AAPMD meeting in Puerto Rico due to the hurricane, have added more stress and lost sleep.
All sleep docs should take training in Mindfulness. I thought I would tune up my efforts, and contacted my friend, Mark Abramson, DDS, inventor of the OASYS sleep appliance, and a Mindfulness instructor. Meditation at Stanford Medical School. He will be offering a course on Mindfulness for Dentists at University of Maryland School of Dentistry, October 28th. I plan on being there.
If we are to offer collaborative care for airway problems we should treat ourselves first. It will make us healthier, more understanding and better practitioners.

